We're loading the full news article for you. This includes the article content, images, author information, and related articles.
The Ministry of Health is transitioning to a single-dose Human Papillomavirus (HPV) vaccine regimen, a strategic shift backed by local research to enhance accessibility and accelerate the elimination of cervical cancer, which claims at least nine Kenyan women daily.
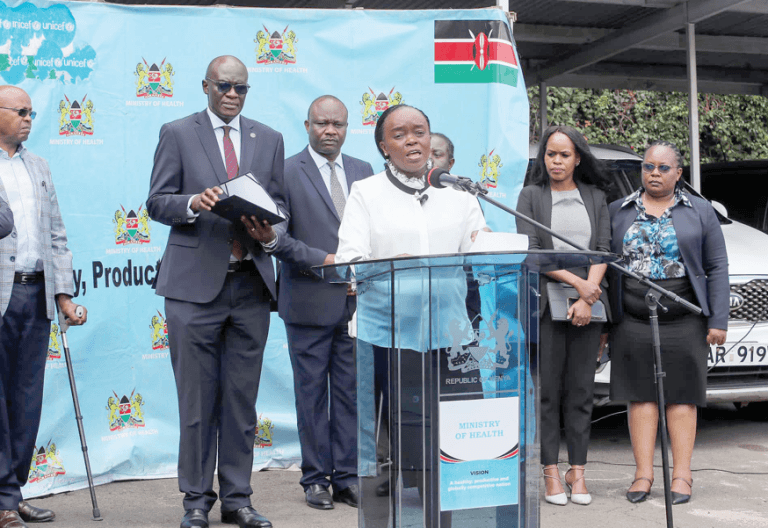
The Kenyan Ministry of Health announced on Wednesday, October 22, 2025, its decision to adopt a single-dose Human Papillomavirus (HPV) vaccine schedule, moving away from the previous two-dose regimen. This significant policy change, set to be rolled out in the coming weeks, is informed by robust local data indicating that a single dose offers comparable protection against the virus responsible for the majority of cervical cancer cases.
Dr. Patrick Amoth, the Director-General for Health, highlighted this as a major milestone in evidence-based innovation during the National Science Research Translation Congress at the African Population and Health Research Center (APHRC) campus in Nairobi. He emphasised that the shift will make vaccination more accessible, affordable, and sustainable across Kenya.
Kenya first introduced a two-dose HPV vaccination programme in October 2019, targeting 10-year-old girls. While first-dose coverage among girls aged 10-14 years rose from 24% in 2022 to over 60% by the end of 2024, the uptake of the second dose consistently lagged. For instance, by 2021, approximately 77% of eligible girls received the first dose, but only 31% completed both doses. This gap underscored the challenges of ensuring follow-up for multiple doses in a low-resource setting.
Cervical cancer remains a critical public health challenge in Kenya, ranking as the second most common cancer among women after breast cancer, and the leading cause of cancer-related deaths among women. Annually, it accounts for an estimated 5,236 new cases and 3,211 deaths, with approximately nine to ten women dying daily from the disease. Without urgent intervention, daily cervical cancer deaths could more than double by 2040.
The decision to transition to a single-dose regimen is strongly supported by the Kenya Single-dose HPV-vaccine Efficacy (KEN SHE) Study. This randomised controlled trial, conducted across Nairobi, Thika, and Kisumu, enrolled 2,275 women aged 15-20 years. The study's findings, presented at the 35th International Papillomavirus Conference, demonstrated that a single dose of both bivalent and nonavalent HPV vaccines offered high efficacy, with approximately 98% protection against persistent HPV infections over three years. This local research, led by Kenyan scientists including Dr. Nelly Mugo and Dr. Maricianah Onono from the Kenya Medical Research Institute (KEMRI), proved that one dose is nearly as effective as traditional multi-dose schedules.
The National Immunisation Technical Advisory Group (NITAG) recommended the single-dose approach, aligning Kenya with over 50 other countries adopting this simplified schedule. This move is in line with the World Health Organization's (WHO) Global Strategy to Eliminate Cervical Cancer, which sets targets of 90% HPV vaccination coverage by age 15, 70% screening coverage at ages 35 and 45, and 90% timely treatment for cervical disease.
The Ministry of Health's commitment to data-driven policy-making underscores this change, with Dr. Amoth stating, “We make policy based on data. Research has to guide every change we make in our immunisation programme.”
The transition is expected to significantly improve vaccine coverage, particularly in underserved areas, and ease the completion of the vaccination schedule for families. The government plans to strengthen strategies to close vaccination gaps by enhancing adolescent-friendly health services, empowering health workers with communication tools, and leveraging data to target communities with low uptake. The school-based vaccination programme is also expanding to reach girls in primary Grade Five, in partnership with the Ministry of Education.
Despite progress, challenges such as safety fears, concerns about side effects, and myths linking the vaccine to infertility persist. These factors contribute to vaccine hesitancy, which Dr. Amoth described as a major public health communication challenge. The Ministry of Health plans to work closely with the media to combat misinformation and build trust in the single-dose strategy.
The successful implementation of the single-dose HPV vaccine will be crucial in determining Kenya's trajectory towards eliminating cervical cancer as a public health problem. Monitoring the increase in vaccination rates, particularly in previously hard-to-reach populations, will be key. The government's continued investment in community education and health worker training will also be vital in addressing vaccine hesitancy and ensuring sustained uptake.
Keep the conversation in one place—threads here stay linked to the story and in the forums.
Other hot threads
E-sports and Gaming Community in Kenya
Active 8 months ago
The Role of Technology in Modern Agriculture (AgriTech)
Active 8 months ago
Popular Recreational Activities Across Counties
Active 8 months ago
Investing in Youth Sports Development Programs
Active 8 months ago